Surgical Expertise
Surgical Expertise
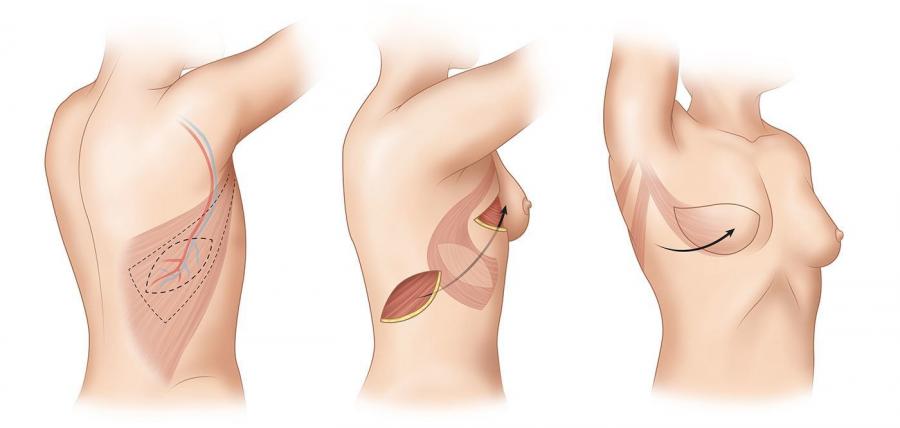
Mastectomy
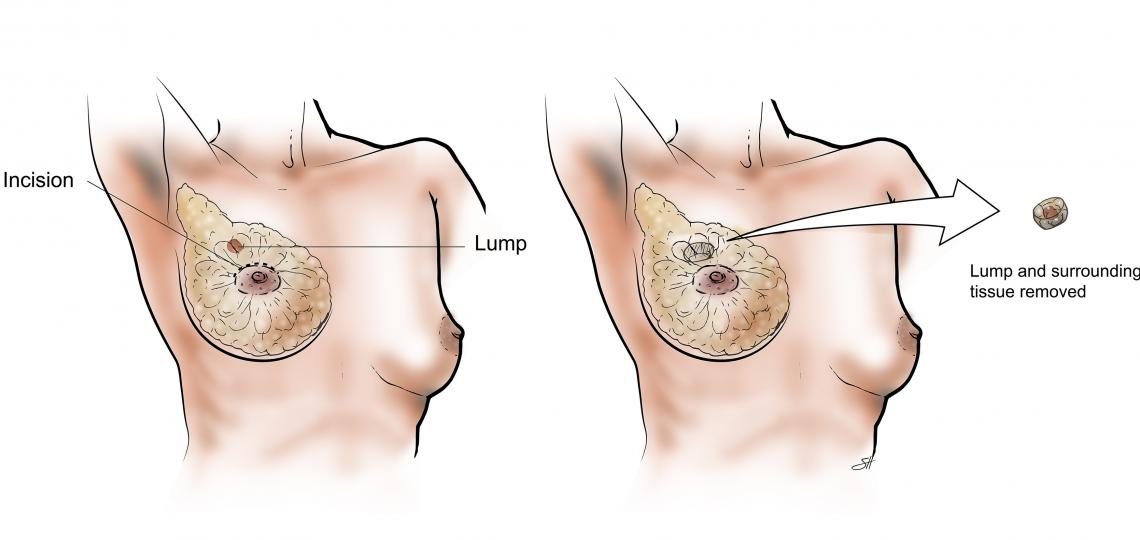
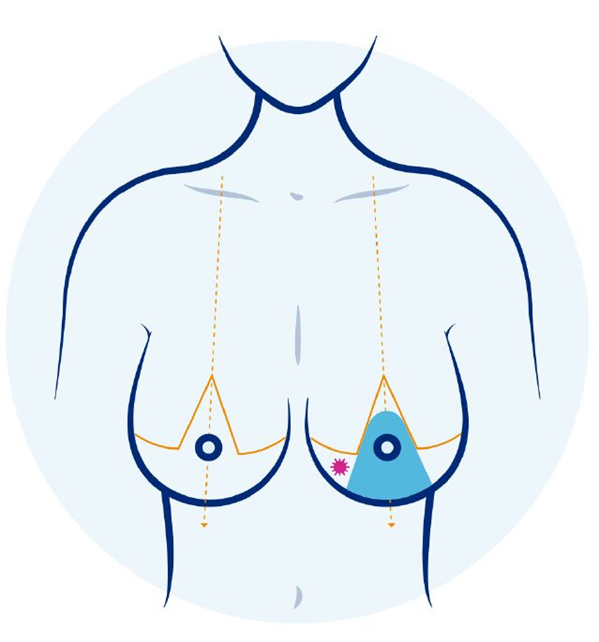
Breast Conservation Surgery (BCS)
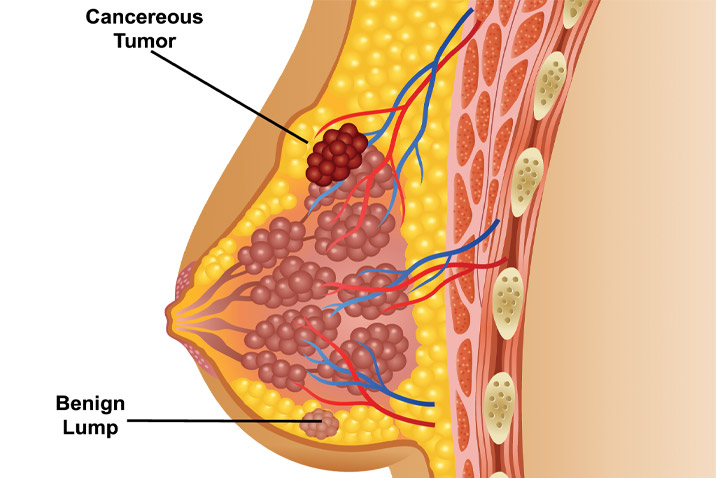
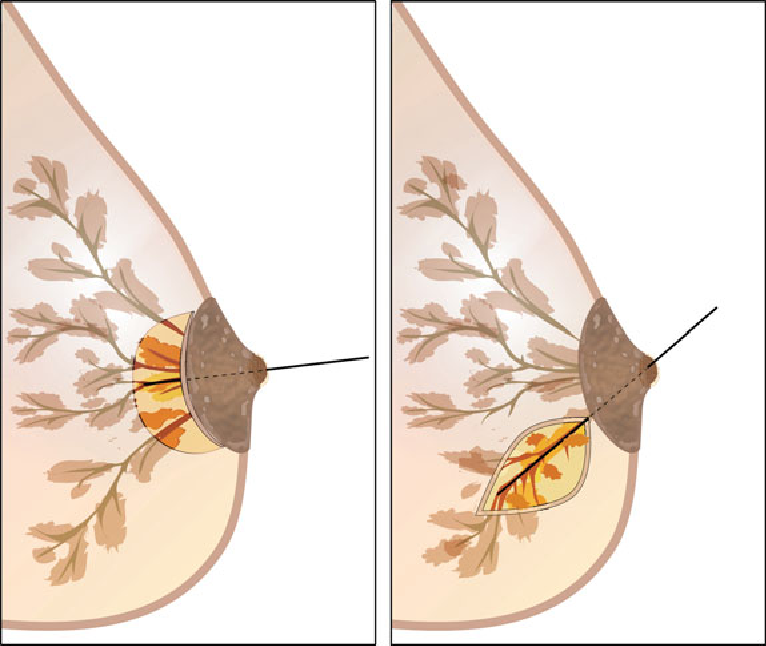
This term is used to describe a surgical technique where the tumour is removed with a margin of normal tissue around it. The margin is checked using frozen section (rapid technique) intraoperatively to ensure that it is tumour free. Along with this ‘lumpectomy’, the axillary lymph nodes are addressed separately using either sentinel lymph node biopsy or complete axillary dissection.
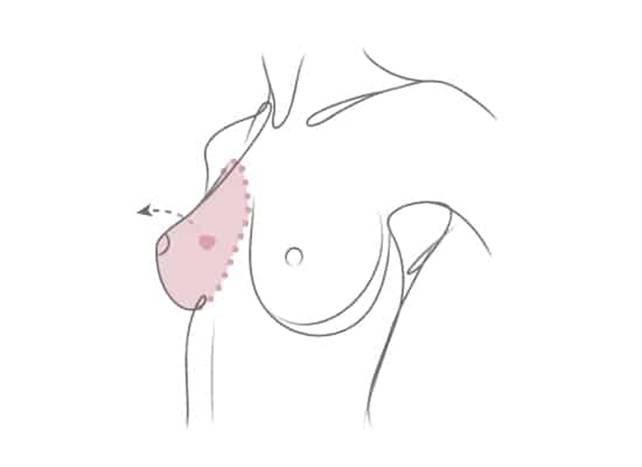
Breast Conservation Surgery is safe with acceptable local recurrence rates compared to mastectomy. It allows a woman to be tumour free while saving her breast and body image. generally, BCS is accompanied by oncoplasty- a procedure to ensure that the size and shape of breast are well maintained. However, radiation therapy for 3-5 weeks is compulsory after breast conservation surgery
BCS is possible in most cases of early breast cancer and even in certain cases of locally advanced disease after neoadjuvant therapy.
It is contraindicated in inflammatory breast cancer or in patients who cannot take radiation therapy. In cases with more than one tumour, the surgical decision making has to be individualised.
Sentinel Lymph Node Biopsy (SLNB)
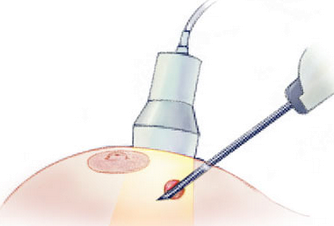
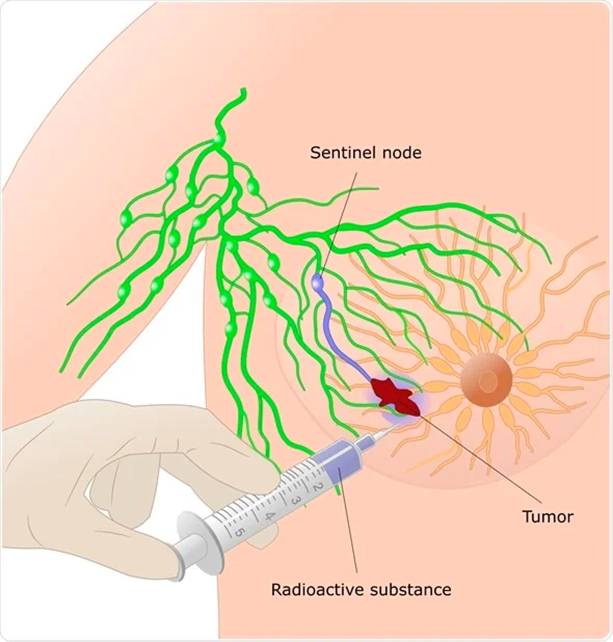
SLNB is a surgical procedure in which the first draining lymph node is identified and removed. Traditionally, in breast cancer patients undergoing surgery, all axillary lymph nodes were removed. This leads to potential shoulder stiffness, numbness and possibility of lymphedema(arm swelling). To decrease this morbidity, now sentinel lymph node biopsy is done for patients with node negative breast cancer and in certain, post chemotherapy cases.
In this technique, 2 dyes are used to select the first draining nodes which are then removed and sent for rapid testing called frozen section. The decision to remove further lymph nodes depend on whether cancer has involved the sentinel lymph node or not. This helps us in improving quality of life of our patients without compromising their oncological safety.